Mask Charade
Mask mandates are being used to cover up the reality that GOVERNMENTS, SCHOOLS AND BUSINESS OWNERS HAVE FAILED TO INSTALL THE HVAC EQUIPMENT THAT COULD KEEP ALL OF US SAFE.
SHARE THIS LINK: http://MaskCharade.com
Questions? Want to help? Do you have ideas to share? Contact James Roguski via phone, text, Signal, Telegram or WhatsApp +1 310-619-3055
Download the PDF below, print it out and distribute the simple flyers to every business you possibly can.
Please watch the video below…
If anyone attempts to require you to wear a mask, please share this website with them:
SHARE THIS LINK: http://MaskCharade.com
There is an enormous amount of scientific evidence available on this topic. I realize that this is a very long article. It is meant to be a resource so that everyone in the world can “follow the science.”
The research collected in this article clearly documents WHY mask mandates must be stopped immediately and permanently.
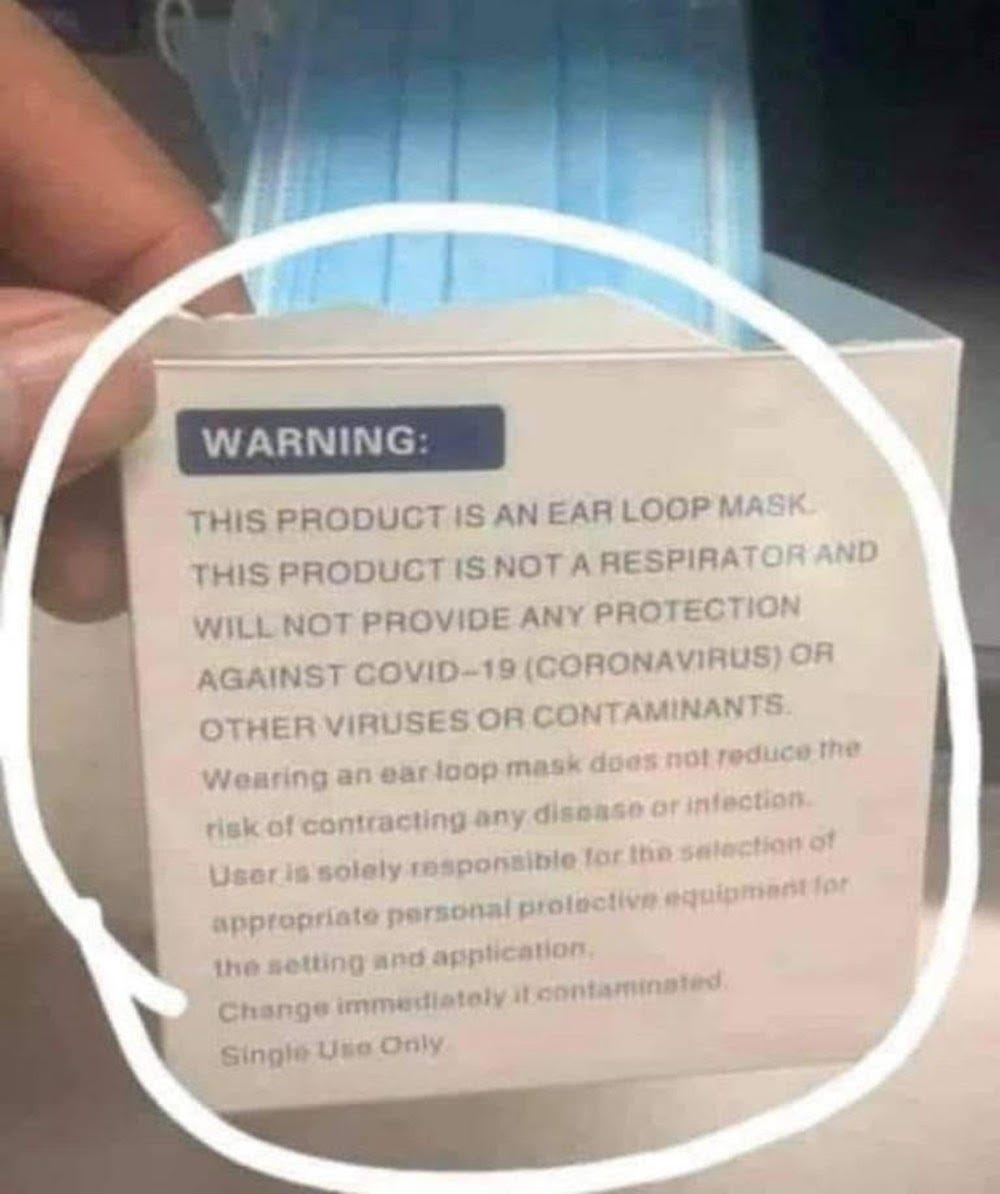
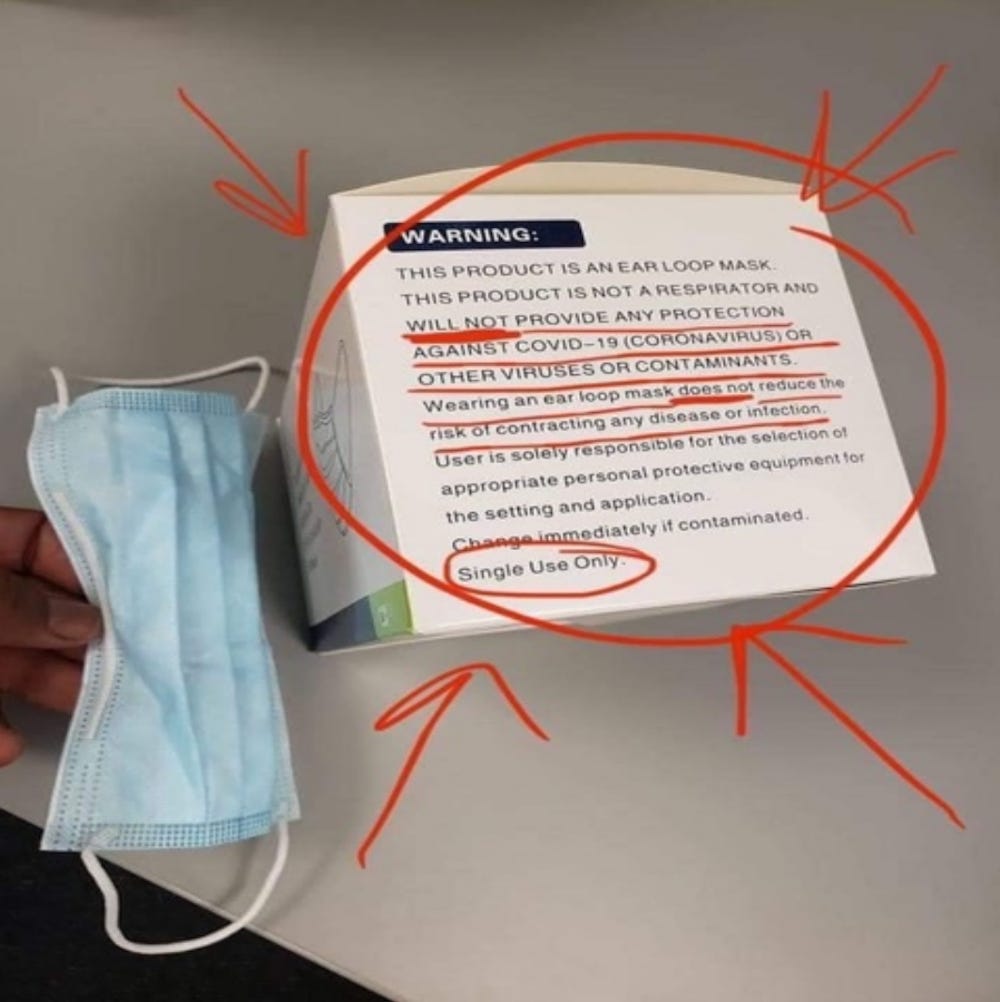
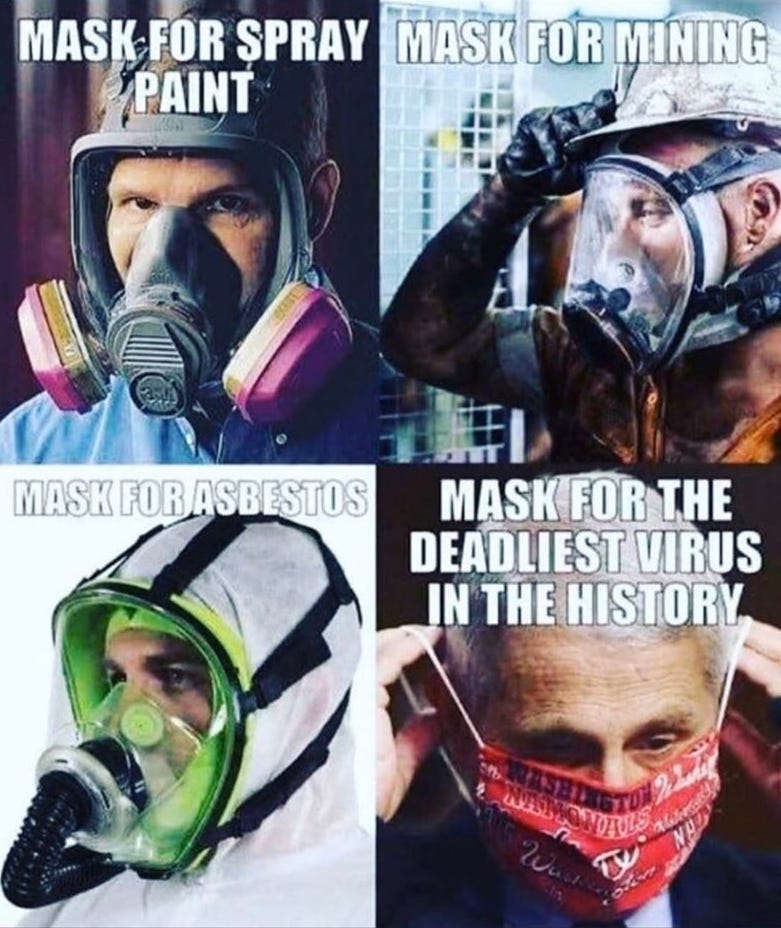
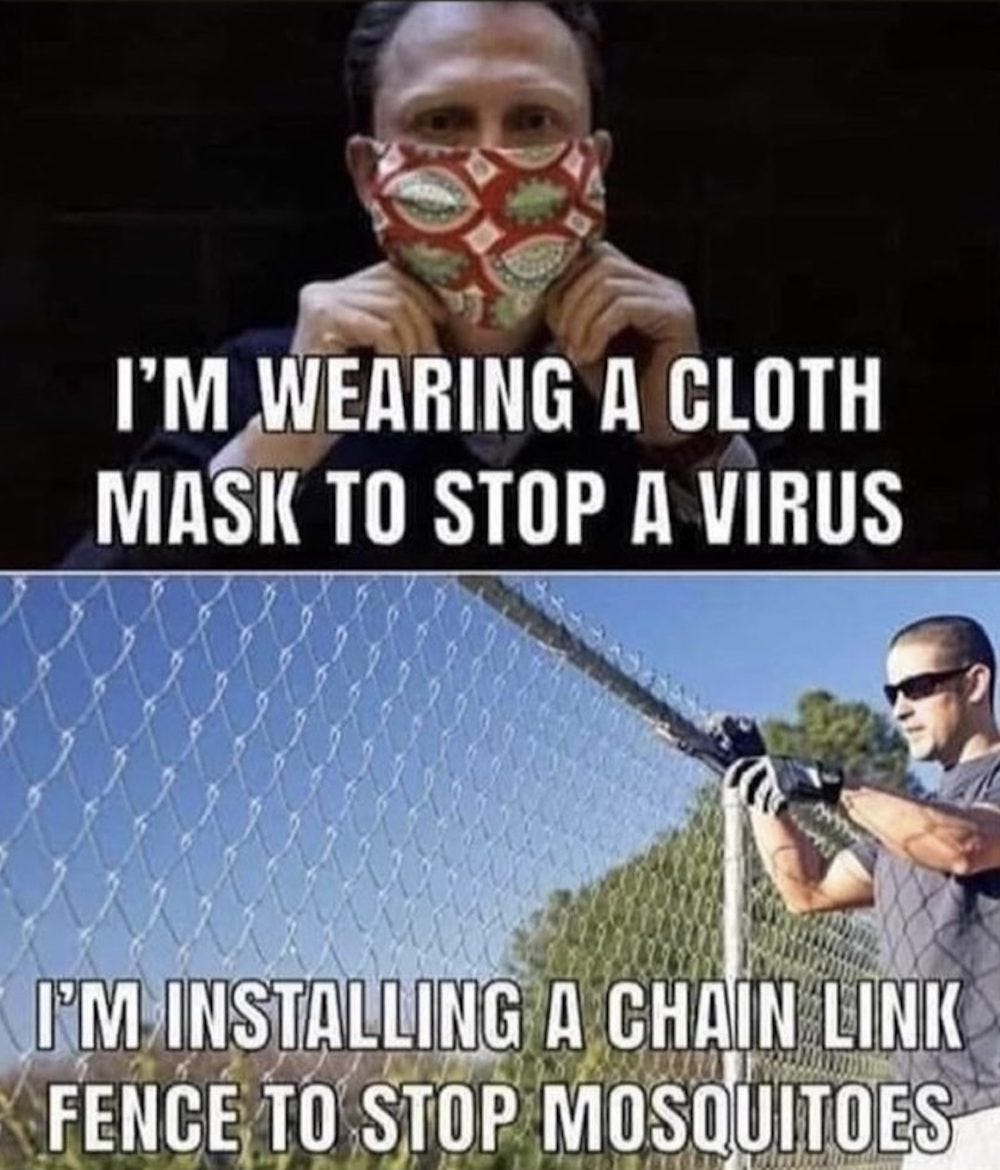
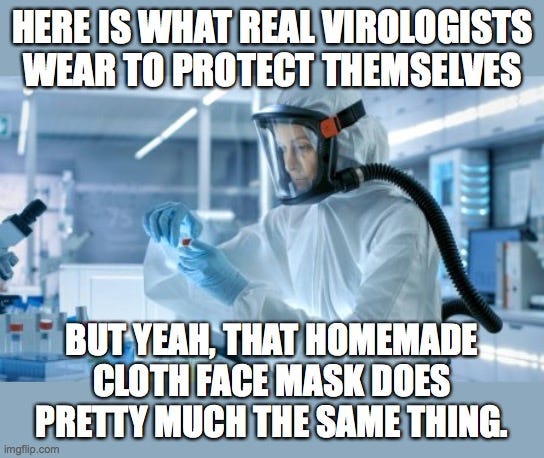
Masks do NOT work.
Masks cause enormous harm.
Mask mandates are being used to cover up an enormous failure of nearly every aspect of our society.
We must ALL work together to raise everyone’s awareness that people in government, business, transportation, schools and universities have failed to install the Heating, Ventilating and Air Conditioning (HVAC) equipment that would remove aerosolized pathogens that we might breathe in while working, shopping, eating, traveling or learning in their facilities.
DIRTY INDOOR AIR CANNOT BE PURIFIED WITH MASKS.
WE CANNOT ALLOW OURSELVES TO BE TORTURED TO MAKE UP FOR THEIR FAILURES TO INSTALL THE HVAC EQUIPMENT THAT WOULD PROTECT EVERYONE.
THEY MUST BE BLAMED AND SHAMED FOR THEIR FAILURES.
Any and all employers, school officials, business owners or other facilities and organizations that attempt to require people to wear masks while performing their job, traveling, attending class, shopping in their store, eating in their restaurant or attending an event are openly admitting that they have failed to install the air purification, circulation and filtration equipment that is necessary to maintain a safe facility.
Every business owner has the moral and ethical responsibility to ensure that they have done everything possible to ensure that the air within their facility has been purified for the safety of their employees and their patrons.
By requiring people to wear masks, they are admitting their failure and their guilt and they are attempting to shift the responsibility onto you, their customer.
THEY HAVE FAILED to install the HVAC equipment that is necessary to clean the indoor air of their facility and they are tacitly admitting that they are operating their business in an unsafe manner.
They should be ashamed of themselves for failing to act and for continuing to operate their business in an unsafe manner. They have literally had years to make the necessary changes, but they have clearly placed profits over the safety of others.
Masks do not work. The research is below.
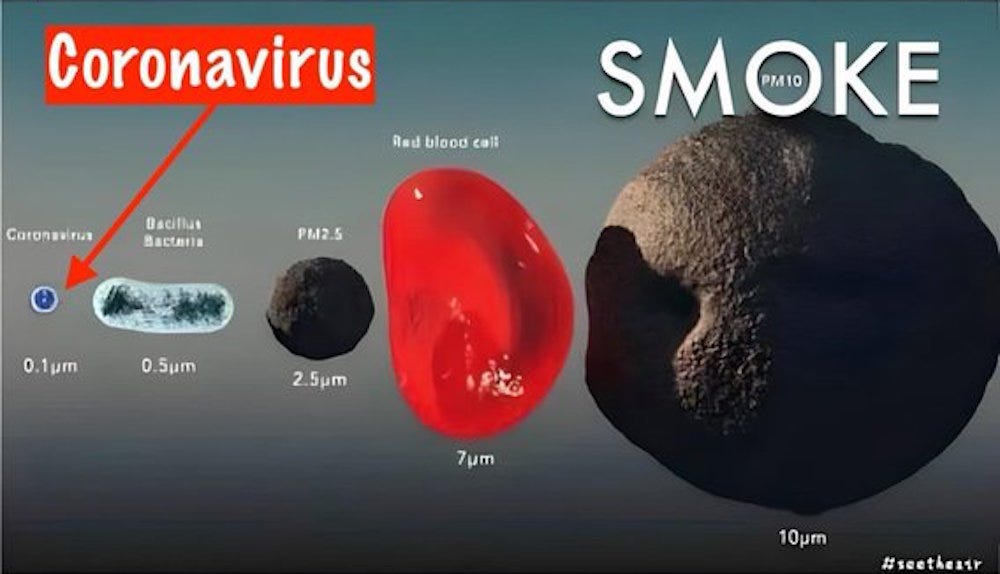
The spaces within all types of masks are too large to effectively filter out aerosolized pathogens.
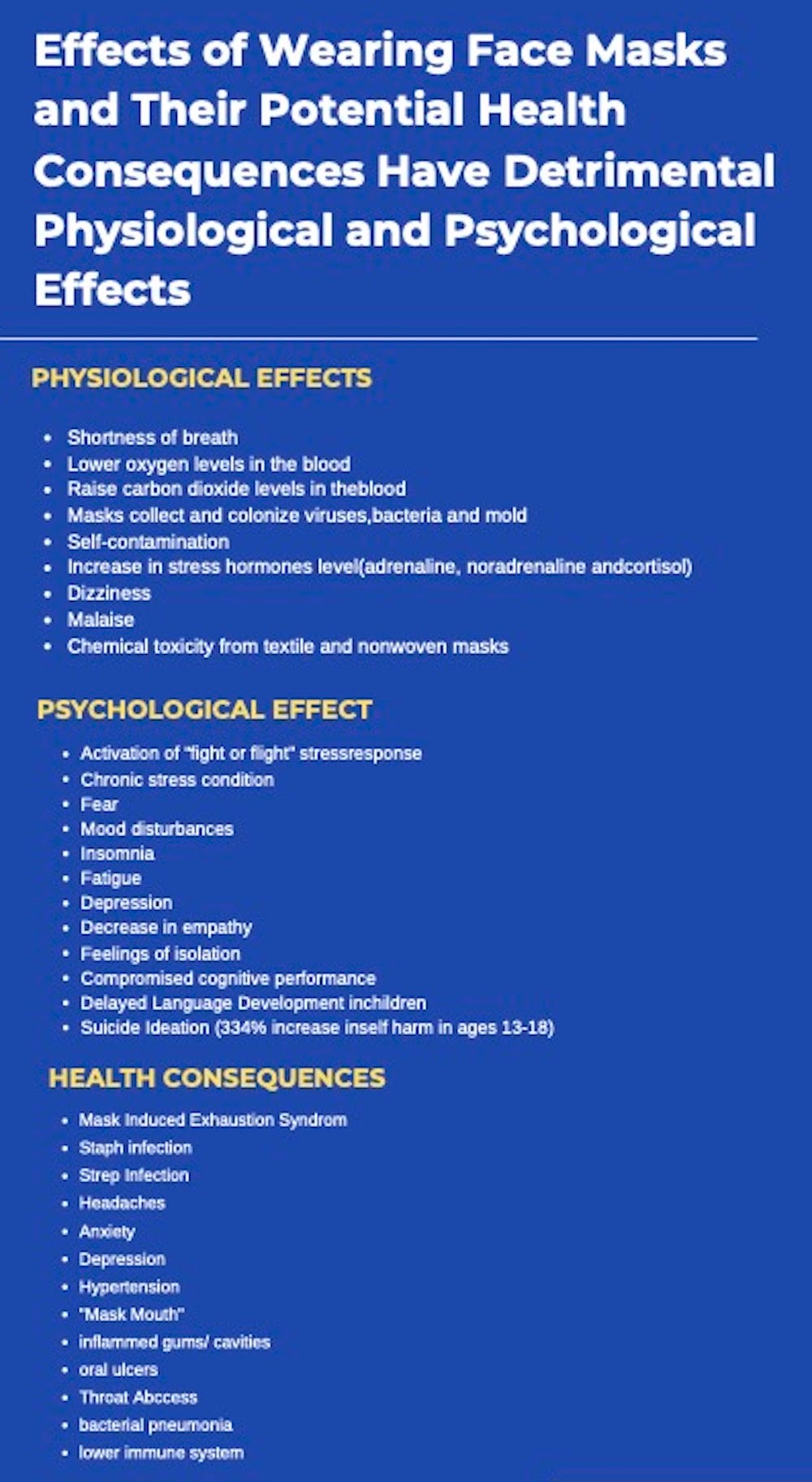
Masks cause harm. The research is below.
Masks cause oxygen deprivation, headaches, anxiety and a wide variety of physical, mental, emotional and psychological ailments.
Masks are merely a control mechanism.
Those who demand that other wear masks are merely attempting to shift blame away from themselves onto other people.
PLEASE WATCH THE VIDEOS BELOW…
Stephen Petty - On the effectiveness of masks
Stephen Petty New Hampshire Legislature Presentation January 27 2022
5.27MB ∙ PDF file
How to Control Exposure to Viruses, Bacteria, and Mold
https://rumble.com/vldll7-how-to-control-exposure-to-viruses-bacteria-and-mold-ep.-06.html
Masks vs. Respirators (What is ACTUALLY PPE) - Ep. 17
https://rumble.com/vlqbee-masks-vs.-respirators-what-is-actually-ppe-ep.-17.html
Dirty Indoor Air
For several decades, dirty indoor air has been implicated in fostering the spread of disease.
To reduce the amount of pathogens and toxic chemicals from indoor spaces, the Federation of European Heating, Ventilation, and Air Conditioning Associations calls for “no use of recirculation,” meaning that fresh outdoor air must be brought in continuously and delivered without mixing with recirculated air. The European group also recommends flushing out buildings for two hours prior to occupancy.
The technologies of air filtration, electrostatic capture, and pathogen dilution and deactivation using techniques such as ultraviolet germicidal irradiation already exist, but they have been ignored.
The overwhelming number of business owners have FAILED to implement these workable strategies.
MASKS WILL NEVER SOLVE THE PROBLEM OF CONTAMINATED INDOOR AIR.
Never before has it been so important for you to stand up for your rights! Mandatory medicine and mandated interventions such as social distancing and mask-wearing have no place in a free society. We, the people, have the right to make responsible decisions about what is best for ourselves and our children based on our own unique circumstances.
Measures that are meant to protect the community as a whole are abhorrent if they hurt individuals in that community.
It is unethical and unconstitutional to force healthy citizens to abide by measures that can result in physical and emotional harm, and that trample on their ability to move freely throughout society without discrimination.
For those with deeply held religious beliefs, mask mandates violate their ability to abide by natural law and follow their convictions to walk in faith, not fear. As such, the decision to wear a mask is a highly personal one and may not be universally mandated.
Please watch the video below…
Click on the button below to send an email to your state representatives.
https://StandForHealthFreedom.com/action/no-mask
Frequently Asked Questions:
https://standforhealthfreedom.com/wp-content/uploads/2023/08/Face-Mask-FAQ_August-23-3.pdf
Download the PDF below, print out some copies of the above graphic and share them far and wide.
There is an enormous amount of evidence listed below that documents, beyond any shadow of a doubt, that masks do NOT work.
In fact, masks cause enormous harm.
If you see ANYONE wearing a mask, please share this information with them: MaskCharade.com
Dr. John Campbell - Masks, no evidence they work
“The pooled results of [Randomized Controlled Trials] RCTs did not show a clear reduction in respiratory viral infection with the use of medical/surgical masks. There were no clear differences between the use of medical/surgical masks compared with N95/P2 respirators in healthcare workers when used in routine care to reduce respiratory viral infection.”
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006207.pub6/full
Dr. Anthony Fauci on masks
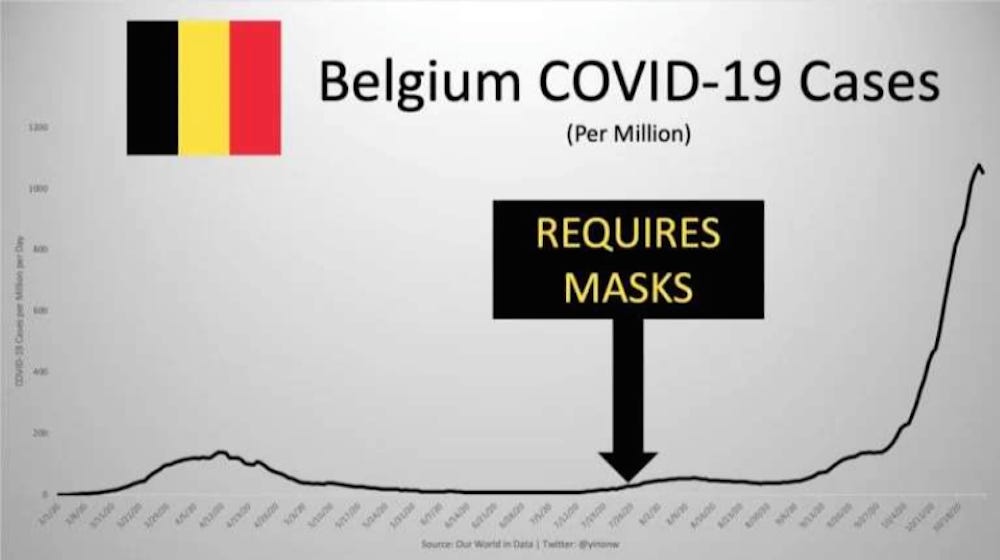
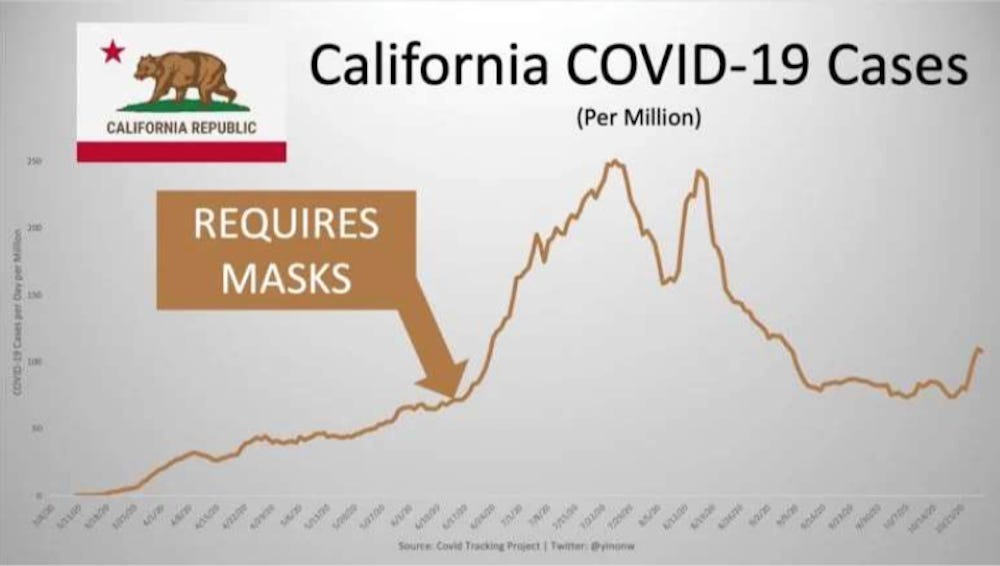
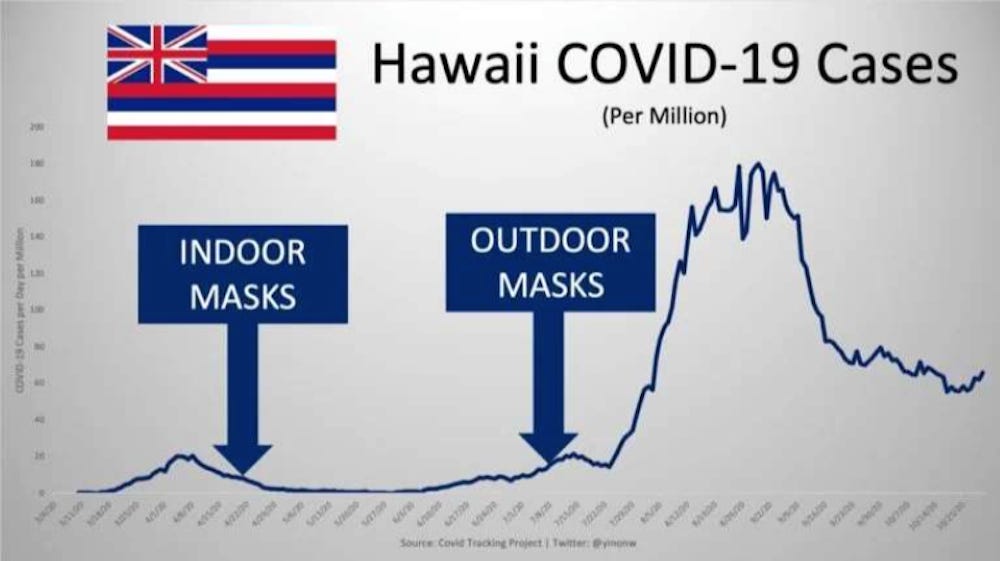
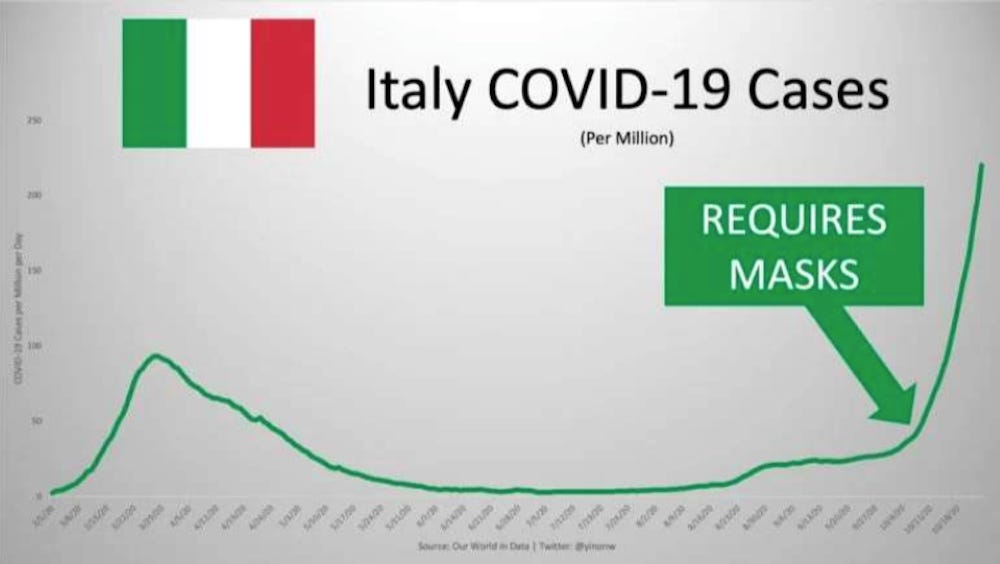
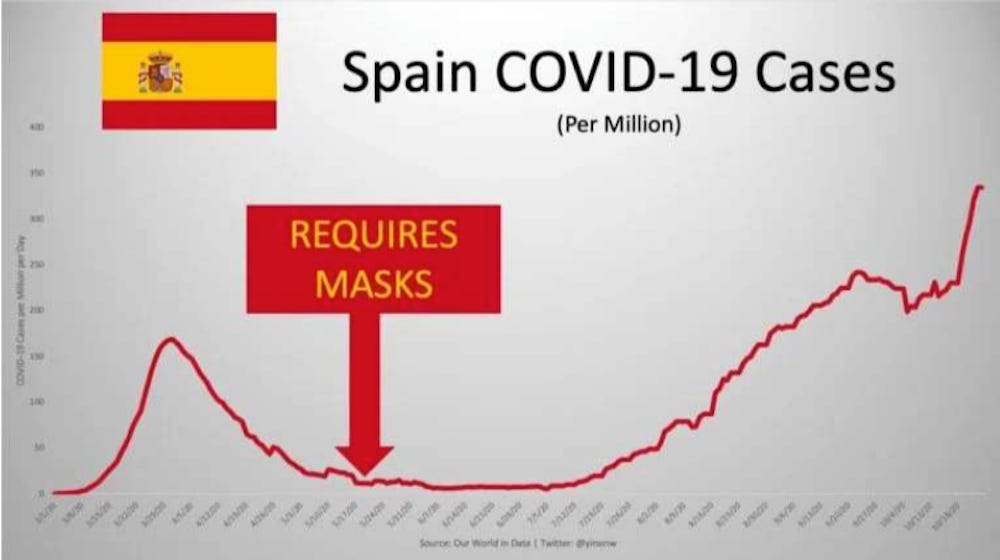
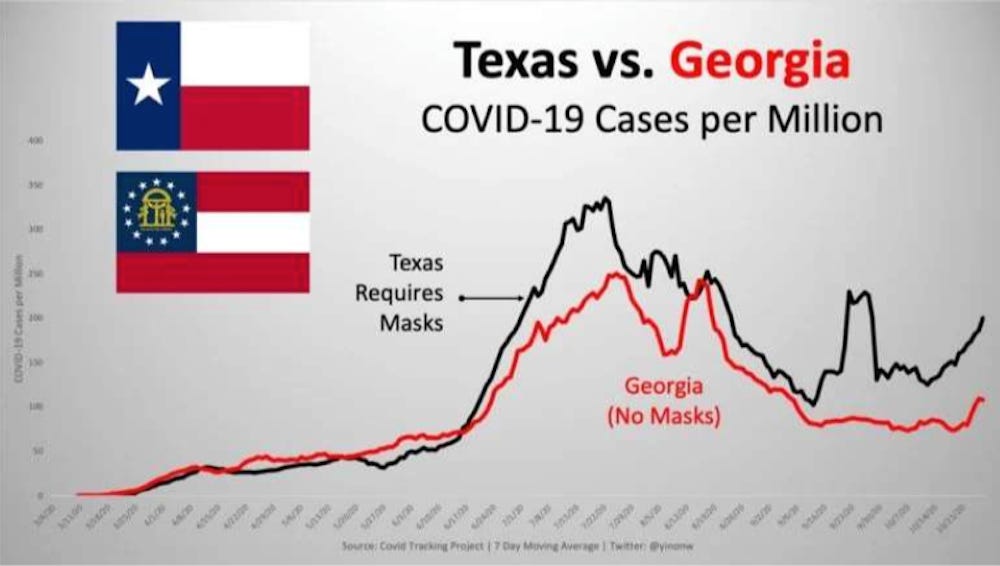
FOLLOW THE DATA…
SOURCE:
https://swprs.org/face-masks-evidence/
Masks Did Not Stop Transmission
3.3MB ∙ PDF file
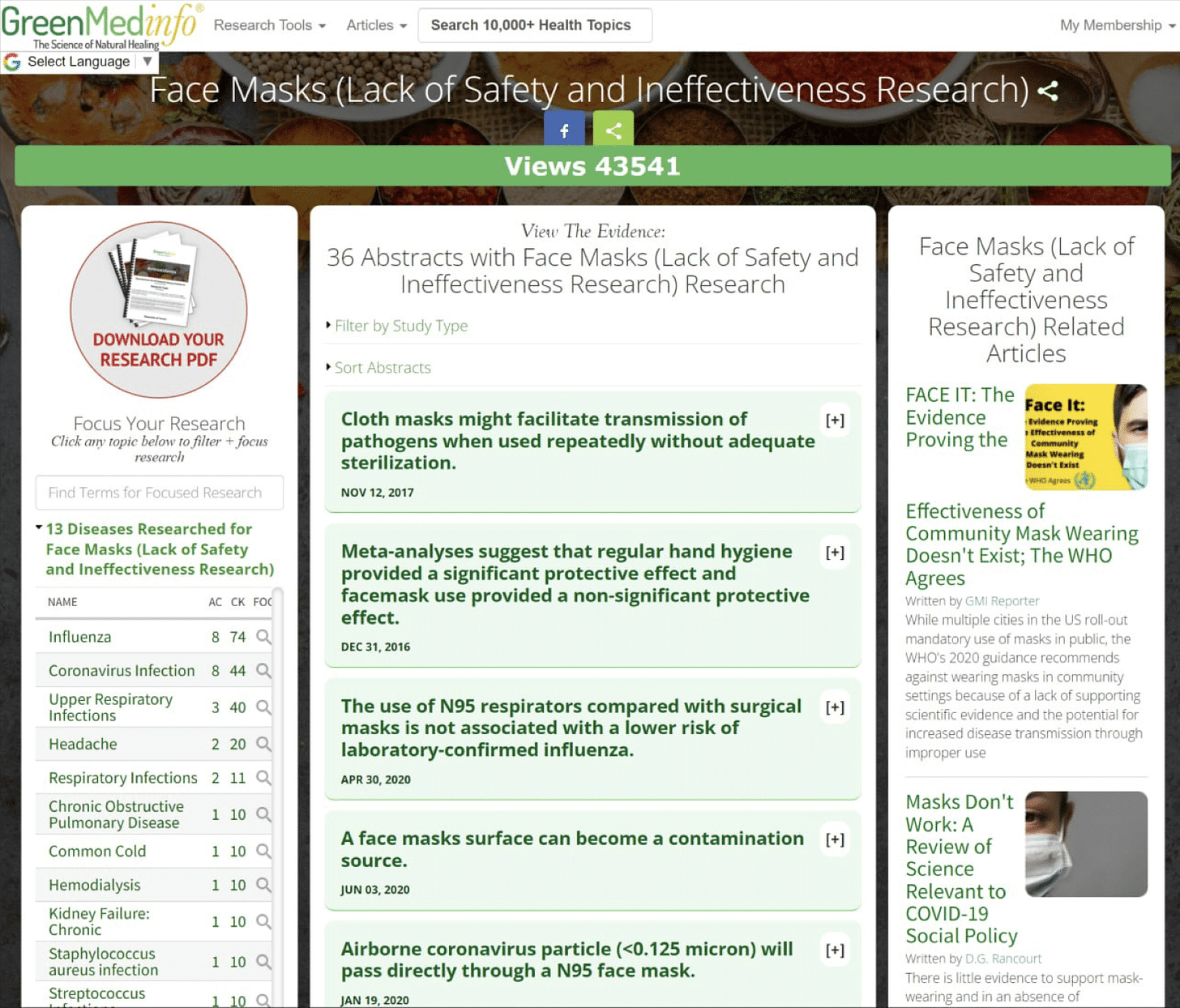
READ THE STUDIES
Below are dozens of published studies providing directly-relevant evidence that face masks do NOT inhibit the spread of respiratory viral infections.
SOURCE:
https://greenmedinfo.com/anti-therapeutic-action/face-masks-lack-safety-and-ineffectiveness-research
SOURCE:
https://childrenshealthdefense.org/community-forum/its-time-to-follow-the-science-masks/
https://aflds.org/medical/masks
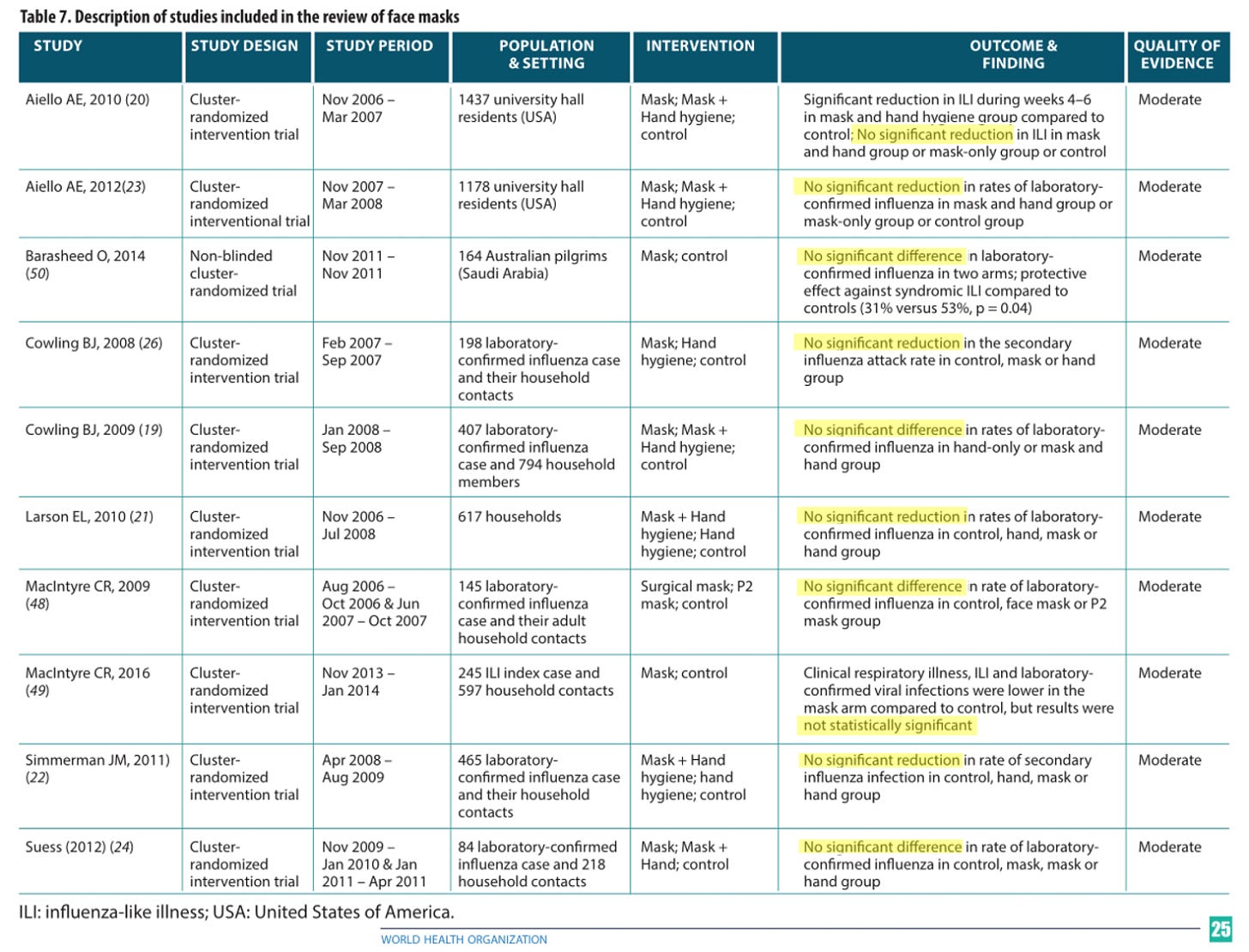
World Health Organization review of face mask trials (2019)
In September 2019, shortly before the coronavirus pandemic, the World Health Organization (WHO) published a comprehensive report on “Non-pharmaceutical public health measures for mitigating the risk and impact of epidemic and pandemic influenza”.
The report reviewed ten randomized controlled trials concerning the effectiveness of face masks against influenza-like illness (ILI). As the following table shows, none of the trials found a statistically significant benefit of face masks.
WHO: 2019 review of face mask RCTs (WHO report/annex)
"We did not find evidence that surgical-type face masks are effective in reducing laboratory-confirmed influenza transmission, either when worn by infected persons (source control) or by persons in the general community to reduce their susceptibility"
Xiao, J., et al., Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings—Personal Protective and Environmental Measures. Emerging Infectious Diseases, 2020. 26(5): p. 967-975.
"The surgical mask seems to provide excellent conditions for the survival of oral or dermal bacteria."
"It was found that when wearing surgical masks for more than 2 hours, an increasing number of microorganisms from the environment or from the oral cavity and respiratory system of the mask wearer accumulate."
"Touching the outer surface of the mask should be avoided at any time. After touching or removing the mask, the hands must be disinfected."
Gund, M., J. Isack, M. Hannig, S. Thieme-Ruffing, B. Gärtner, G. Boros, and S. Rupf. "Contamination of Surgical Mask During Aerosol-Producing Dental Treatments." Clin Oral Investig (Oct 27 2020): 1-8. https://dx.doi.org/10.1007/s00784-020-03645-2.
Zhiqing, L., C. Yongyun, C. Wenxiang, Y. Mengning, M. Yuanqing, Z. Zhenan, W. Haishan, Z. Jie, D. Kerong, L. Huiwu, L. Fengxiang, and Z. Zanjing. "Surgical Masks as Source of Bacterial Contamination During Operative Procedures." J Orthop Translat 14 (Jul 2018): 57-62. https://dx.doi.org/10.1016/j.jot.2018.06.002.
https://www.sciencedirect.com/science/article/pii/S2214031X18300809
"We included three trials, involving a total of 2106 participants. There was no statistically significant difference in infection rates between the masked and unmasked group in any of the trials" (Vincent et. al., 2016)
Vincent, M. and P. Edwards, Disposable surgical face masks for preventing surgical wound infection in clean surgery. Cochrane Database of Systematic Reviews, 2016.
"In our study regular use of face masks offered no significant protection against ARI [Acute Respiratory Infections]. Our finding is in agreement, however, with the conclusion of the Centers for Disease Control and Prevention (CDC) in the USA which stated that surgical masks are not designed for use as particulate respirators and do not provide much protection against air-borne diseases because they do not effectively filter small particles from the air or prevent leakage around the edge of the mask when the user inhales."
"Furthermore, we found that intermittent use of surgical-type masks was actually associated with more than a 2.5-fold greater risk of infection. It is possible that once a facemask is worn in the presence of an infected patient, the mask could become contaminated with infectious material and touching the outside of the device could result in hand transmission of the infection to the respiratory tract during nose-rubbing."
Aiello, A. E., G. F. Murray, V. Perez, R. M. Coulborn, B. M. Davis, M. Uddin, D. K. Shay, S. H. Waterman, and A. S. Monto. "Mask Use, Hand Hygiene, and Seasonal Influenza-Like Illness among Young Adults: A Randomized Intervention Trial." J Infect Dis 201, no. 4 (Feb 15 2010): 491-8. https://dx.doi.org/10.1086/650396.
https://academic.oup.com/jid/article/201/4/491/861190
Aiello, Allison E., Vanessa Perez, Rebecca M. Coulborn, Brian M. Davis, Monica Uddin, and Arnold S. Monto. "Facemasks, Hand Hygiene, and Influenza among Young Adults: A Randomized Intervention Trial." PLoS One 7, no. 1 (2012): e29744. https://dx.doi.org/10.1371/journal.pone.0029744.
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0029744
"In intention-to-treat analysis, face mask use was neither effective against laboratory-confirmed vRTIs [Viral Respiratory Tract Infections] nor against CRI [Clinical Respiratory Infections], not even in per-protocol analysis."
Barasheed, O., N. Almasri, A. M. Badahdah, L. Heron, J. Taylor, K. McPhee, I. Ridda, E. Haworth, D. E. Dwyer, H. Rashid, and R. Booy. "Pilot Randomised Controlled Trial to Test Effectiveness of Facemasks in Preventing Influenza-Like Illness Transmission among Australian Hajj Pilgrims in 2011." Infect Disord Drug Targets 14, no. 2 (2014): 110-6. https://dx.doi.org/10.2174/1871526514666141021112855.
https://www.eurekaselect.com/article/62953
Wang, M., O. Barasheed, H. Rashid, R. Booy, H. El Bashir, E. Haworth, I. Ridda, E. C. Holmes, D. E. Dwyer, J. Nguyen-Van-Tam, Z. A. Memish, and L. Heron. "A Cluster-Randomised Controlled Trial to Test the Efficacy of Facemasks in Preventing Respiratory Viral Infection among Hajj Pilgrims." J Epidemiol Glob Health 5, no. 2 (Jun 2015): 181-9. https://dx.doi.org/10.1016/j.jegh.2014.08.002.
https://www.atlantis-press.com/journals/jegh/125906011
Alfelali, Mohammad, Elizabeth Haworth, Osamah Barasheed, Al-Mamoon Badahdah, Hamid Bokhary, Mohamed Tashani, Mohammad Azeem, Jen Kok, Janette Taylor, Elizabeth Barnes, Haitham Bashir, Gulam Khandaker, Edward Holmes, Dominic Dwyer, Leon Heron, Godwin Wilson, Robert Booy, and Harunor Rashid. "Facemask Versus No Facemask in Preventing Viral Respiratory Infections During Hajj: A Cluster Randomised Open Label Trial." SSRN Electronic Journal (01/01 2019). https://dx.doi.org/10.2139/ssrn.3349234. (Preprint)
The authors found no statistically significant difference in SARS-CoV-2 infection rates between the masked and non-masked study cohorts.
Bundgaard, H., J. S. Bundgaard, D. E. T. Raaschou-Pedersen, C. von Buchwald, T. Todsen, J. B. Norsk, M. M. Pries-Heje, C. R. Vissing, P. B. Nielsen, U. C. Winsløw, K. Fogh, R. Hasselbalch, J. H. Kristensen, A. Ringgaard, M. Porsborg Andersen, N. B. Goecke, R. Trebbien, K. Skovgaard, T. Benfield, H. Ullum, C. Torp-Pedersen, and K. Iversen. "Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent Sars-Cov-2 Infection in Danish Mask Wearers : A Randomized Controlled Trial." Ann Intern Med 174, no. 3 (Mar 2021): 335-43. https://dx.doi.org/10.7326/m20-6817.
“Strikingly, a detectable level of infectious virus could still be present on the outer layer of a surgical mask on day 7."
Of all the materials tested, SARS-CoV-2 remained viable longest on medical masks.
Findings show that SARS-CoV-2 remains viable longer on the inner and outer layer of medical masks than on most other common materials.
Compares the length of time SARS-CoV-2 remains infectious on various surface materials.
Compared viability duration of SARS-CoV-2 on paper, tissue paper, wood, cloth, glass, banknotes, stainless steel, plastic, mask inner layer, and mask outer layer.
"No infectious virus could be recovered from printing and tissue papers after a 3-hour incubation, whereas no infectious virus could be detected from treated wood and cloth on day 2. By contrast, SARS-CoV-2 was more stable on smooth surfaces. No infectious virus could be detected from treated smooth surfaces on day 4 (glass and banknote) or day 7 (stainless steel and plastic).”
Masks are not useful in preventing the spread of SARS-CoV-2, and may even have a detrimental effect by extending the viral period of viability.
Chin, A. W. H., J. T. S. Chu, M. R. A. Perera, K. P. Y. Hui, H. L. Yen, M. C. W. Chan, M. Peiris, and L. L. M. Poon. "Stability of Sars-Cov-2 in Different Environmental Conditions." Lancet Microbe 1, no. 1 (May 2020): e10. https://dx.doi.org/10.1016/s2666-5247(20)30003-3.
https://www.thelancet.com/journals/lanmic/article/PIIS2666-5247(20)30003-3/fulltext
"... we did not find any evidence of decreased risk of transmission in individuals who reported mask use."
Marks, M., et al., Transmission of COVID-19 in 282 clusters in Catalonia, Spain: a cohort study. The Lancet Infectious Diseases, 2021.
https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30985-3/fulltext
"Cloth masks resulted in significantly higher rates of infection than medical masks, and also performed worse than the control arm."
"Observations during SARS suggested double-masking and other practices increased the risk of infection because of moisture, liquid diffusion and pathogen retention."
"...we compared rates of infection in the medical mask arm with rates observed in medical mask arms from two previous RCTs in which no efficacy of medical masks could be demonstrated when compared with control or N95 respirators."
"the rate of virus isolation in the no-mask control group in the first Chinese RCT was 3.1%, which was not significantly different to the rates of virus isolation in the medical mask arms in any of the three trials including this one."
"... the magnitude of difference raises the possibility that cloth masks cause an increase in infection risk in HCWs."
"The rates of all infection outcomes were highest in the cloth mask arm.... and the results caution against the use of cloth masks."
MacIntyre, C. R., H. Seale, T. C. Dung, N. T. Hien, P. T. Nga, A. A. Chughtai, B. Rahman, D. E. Dwyer, and Q. Wang. "A Cluster Randomised Trial of Cloth Masks Compared with Medical Masks in Healthcare Workers." BMJ Open 5, no. 4 (Apr 22 2015): e006577. https://dx.doi.org/10.1136/bmjopen-2014-006577.
"We found that with the element of aspiration introduced, as in the natural use of masks, even five layers did not give a sufficient reduction in count to make such a mask of value."
The authors of this study used a proxy organism (Bacillus prodigiosus, also known as Serratia marcescens) which are typically 500 to 2,000 nanometers - many times the size of the 60-140nm SARS-CoV-2 virus.
Kellogg, W. H., and Grace Macmillan. "An Experimental Study of the Efficacy of Gauze Face Masks." American Journal of Public Health 10, no. 1 (1920): 34-42. https://dx.doi.org/10.2105/ajph.10.1.34.
Meta-Analysis of Randomized Control Trials
Ioannidis, J.P.A., Reconciling estimates of global spread and infection fatality rates of COVID-19: An overview of systematic evaluations. European Journal of Clinical Investigation, 2021.
Xiao, J., et al., Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings—Personal Protective and Environmental Measures. Emerging Infectious Diseases, 2020. 26(5): p. 967-975
Smith, J.D., et al., Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis. Cmaj, 2016. 188(8): p. 567-574.
Saunders-Hastings, P., et al., Effectiveness of personal protective measures in reducing pandemic influenza transmission: A systematic review and meta-analysis. Epidemics, 2017. 20: p. 1-20.
Offeddu, V., et al., Effectiveness of Masks and Respirators Against Respiratory Infections in Healthcare Workers: A Systematic Review and Meta-Analysis. Clin Infect Dis, 2017. 65(11): p. 1934-1942.
Long, Y., et al., Effectiveness of N95 respirators versus surgical masks against influenza: A systematic review and meta-analysis. J Evid Based Med, 2020. 13(2): p. 93-101.
Jefferson, T., et al., Physical interventions to interrupt or reduce the spread of respiratory viruses. part 1 - face masks, eye protection and person distancing: systematic review and meta-analysis. 2020, Cold Spring Harbor Laboratory
Vincent, M. and P. Edwards, Disposable surgical face masks for preventing surgical wound infection in clean surgery. Cochrane Database of Systematic Reviews, 2016.
Lipp, A. and P. Edwards, Disposable surgical face masks for preventing surgical wound infection in clean surgery. Cochrane Database of Systematic Reviews, 2014.
Bartoszko, J.J., et al., Medical masks vs N95 respirators for preventing COVID-19 in healthcare workers: A systematic review and meta-analysis of randomized trials. Influenza Other Respir Viruses, 2020. 14(4): p. 365-373.
Mask Non Efficacy Reference Table
738KB ∙ PDF file
https://www.realmaskscience.com/references
MASKS CAUSE SIGNIFICANT HARM
OSHA requires an initial respirator fit test to identify the right model, style, and size respirator for each worker in addition to annual fit tests. Additionally, tight-fitting respirators, including the N95, require a user seal check each time one is put on. Facial hair at the sealing area of the respirator will cause it to leak.
Respirators require a medical evaluation before use because they can make breathing more difficult. Some conditions that could prevent respirator use include heart conditions, lung disease, and psychological conditions such as claustrophobia.
In laboratories at biosafety level 2 and higher, respirators are recommended to be discarded as hazardous waste after a single use.
Dr. Christina Parks
https://rumble.com/v1xqhu8-dr.-christina-parks-aflih-summit-2022.html
Dr. Michael Gaeta
https://www.bitchute.com/video/vYkfKETdnYye/
Order the flyers below and distribute them widely.
https://citizensforfreespeech.store/shop/free_speech/dr-blaylock-brochures/
Real Mask Science Poster
Mask Side Effects Poster
5.15MB ∙ PDF file
https://www.realmaskscience.com/references
The mandatory masking of children is TORTURE.
Protection of the Educational Rights of Kids (PERK) provides a wealth of information. Please visit their website for information, in addition to the PDFs provided below…
https://www.PERK-group.com/masks-harm-children
Masks are Unnecessary (DOWNLOAD PDF)
Masks are Ineffective (DOWNLOAD PDF)
Masks Harm Children (DOWNLOAD PDF)
Longterm Use of Facemasks are Harmful (DOWNLOAD PDF)
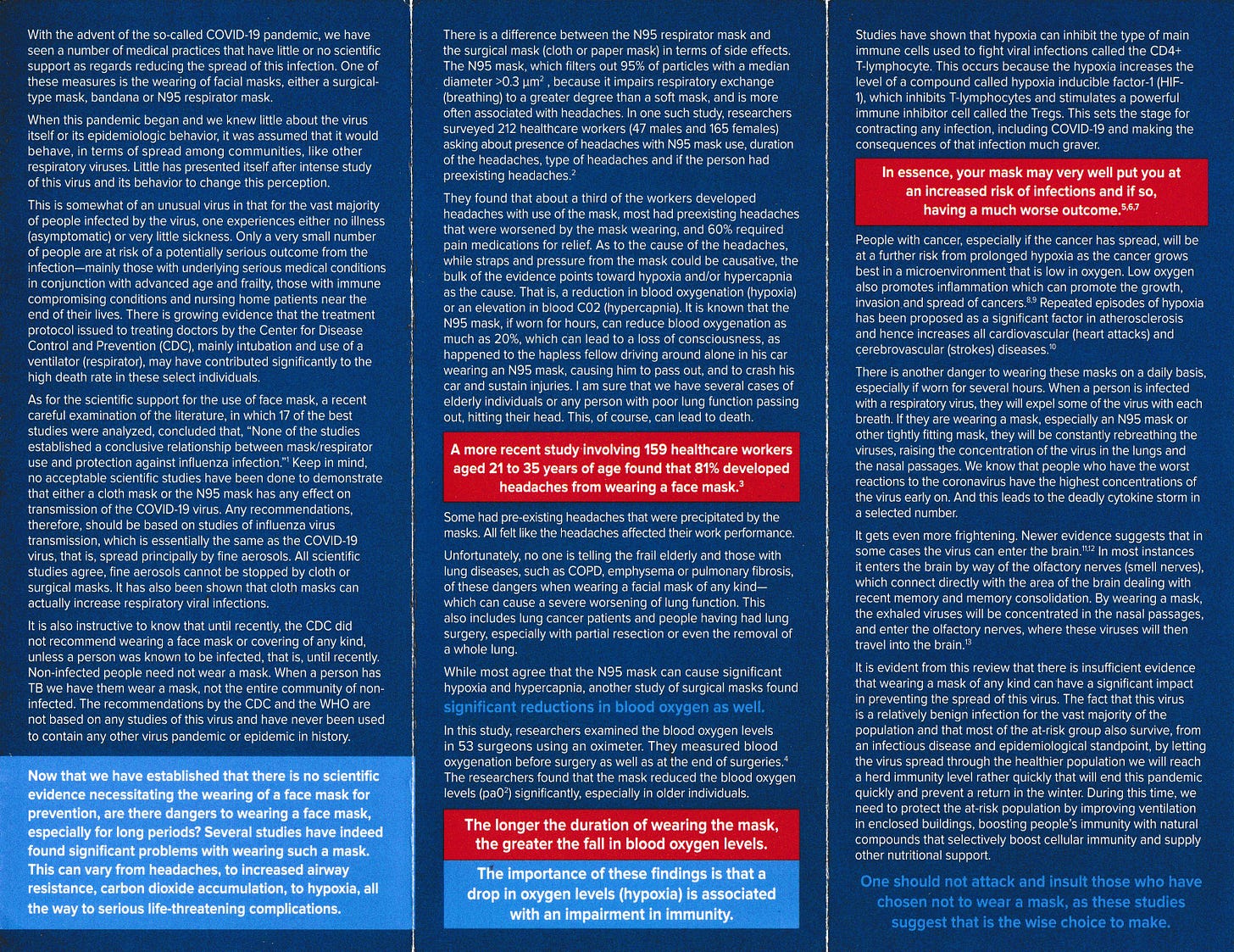
Excerpts from the WHO Interim Guidance Document:
Wearing masks for a prolonged period of time may cause harm, as the following evidence shows:
The WHO warns of various “side effects”such as difficulty breathing and skin rashes.
A Japanese study, published in Nature Scientific Reports, found a significant number of bacteria and fungi on face masks, including some pathogenic microbes.
An Israeli-Canadian study, published in Cognitive Research in February 2022, found that “face masks disrupt holistic processing and face perception in school-age children”.
Tests conducted by the University Hospital of Leipzig in Germany have shown that face masks significantly reduce the resilience and performance of healthy adults.
A German psychological study with about 1000 participants found “severe psychosocial consequences” due to the introduction of mandatory face masks in Germany.
An Italian study using real-time capnography found that face masks and N95/FFP2 masks increased CO2 levels in inhaled air to levels above the acceptable exposure threshold.
The Hamburg Environmental Institutewarned of the inhalation of chlorine compounds in polyester masks as well as problems in connection with face mask disposal.
The European rapid alert system RAPEXhas already recalled over 100 mask models because they did not meet EU quality standards and could lead to “serious risks”.
A study by the University of Muenster in Germany found that on N95 (FFP2) masks, Sars-CoV-2 may remain infectious for several days, thus increasing the risk of self-contamination.
In China, several children who had to wear a mask during gym classes fainted and died; autopsies found a sudden cardiac arrest as the probable cause of death. In the US, a car driver wearing an N95 (FFP2) mask fainted and crasheddue to CO2 intoxication.
SOURCE:
https://swprs.org/face-masks-evidence/
Respiratory/Cardiovascular Burden
Dyspnea, decreased oxygen, increased carbon dioxide, increased respiratory rate, increased airflow resistance, increased blood pressure, and increased heart rate.
1. Beder, A., et al., Preliminary report on surgical mask induced deoxygenation during major surgery. Neurocirugía, 2008. 19(2): p. 121-126.
2. Bharatendu, C., et al., Powered Air Purifying Respirator (PAPR) restores the N95 face mask induced cerebral hemodynamic alterations among Healthcare Workers during COVID-19 Outbreak. Journal of the Neurological Sciences, 2020. 417: p. 117078.
3. Butz, U., Rückatmung von Kohlendioxid bei Verwendung von Operationsmasken als hygienischer Mundschutz an medizinischem Fachpersonal [Rebreathing of carbon dioxide of surgical staff using hygienic masks], in Fakultät für Medizin der Technischen Universität München, Munich, Germany, 2005. 2005, Institute for Anaesthesiology at the Technical University of Munich: Universitätsbibliothek der Technischen Universität München p. 55.
4. Chandrasekaran, B. and S. Fernandes, "Exercise with facemask; Are we handling a devil's sword?" - A physiological hypothesis. Med Hypotheses, 2020. 144: p. 110002.
5. Chao, F.-L., Adolescents’ face mask usage and contact transmission in novel Coronavirus. Journal of Public Health Research, 2020. 9(1).
6. Epstein, D., et al., Return to training in the COVID-19 era: The physiological effects of face masks during exercise. Scandinavian Journal of Medicine & Science in Sports, 2021. 31(1): p. 70-75.
7. Fikenzer, S., et al., Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity. Clin Res Cardiol, 2020. 109(12): p. 1522-1530.
8. Georgi, C., et al., The Impact of Commonly-Worn Face Masks on Physiological Parameters and on Discomfort During Standard Work-Related Physical Effort. Deutsches Arzteblatt international, 2020. 117(40): p. 674-675.
9. Goh, D.Y.T., et al., A randomised clinical trial to evaluate the safety, fit, comfort of a novel N95 mask in children. Scientific Reports, 2019. 9(1).
10. Jagim, A.R., et al., Acute Effects of the Elevation Training Mask on Strength Performance in Recreational Weight lifters. The Journal of Strength & Conditioning Research, 2018. 32(2).
11. Johnson, A.T., Respirator masks protect health but impact performance: a review. Journal of Biological Engineering, 2016. 10(1).
12. Kao, T.W., et al., The physiological impact of wearing an N95 mask during hemodialysis as a precaution against SARS in patients with end-stage renal disease. J Formos Med Assoc, 2004. 103(8): p. 624-8.
13. Kisielinski, K., et al., Is a Mask That Covers the Mouth and Nose Free from Undesirable Side Effects in Everyday Use and Free of Potential Hazards? International Journal of Environmental Research and Public Health, 2021. 18(8): p. 4344.
14. Köseoğlu Toksoy, C., et al., Headache related to mask use of healthcare workers in COVID-19 pandemic. The Korean Journal of Pain, 2021. 34(2): p. 241-245.
15. Kyung, S.Y., et al., Risks of N95 Face Mask Use in Subjects With COPD. Respiratory Care, 2020. 65(5): p. 658-664.
16. Lässing, J., et al., Effects of surgical face masks on cardiopulmonary parameters during steady state exercise. Sci Rep, 2020. 10(1): p. 22363.
17. Li, Y., et al., Effects of wearing N95 and surgical facemasks on heart rate, thermal stress and subjective sensations. International Archives of Occupational and Environmental Health, 2005. 78(6): p. 501-509.
18. Liu, C., et al., Effects of wearing masks on human health and comfort during the COVID-19 pandemic. IOP Conference Series: Earth and Environmental Science, 2020. 531: p. 012034.
19. Matusiak, Ł., et al., Inconveniences due to the use of face masks during the COVID-19 pandemic: A survey study of 876 young people. Dermatologic Therapy, 2020. 33(4).
20. Mo, Y., et al., Risk and impact of using mask on COPD patients with acute exacerbation during the COVID-19 outbreak: a retrospective study. 2020, Research Square.
21. Passali, D., et al., Effects of a Mask on Breathing Impairment During a Fencing Assault: A Case Series Study. Asian Journal of Sports Medicine, 2015. 6(3).
22. Person, E., et al., [Effect of a surgical mask on six minute walking distance]. Rev Mal Respir, 2018. 35(3): p. 264-268.
23. Pifarré, F., et al., COVID-19 and mask in sports. Apunts Sports Medicine, 2020. 55(208): p. 143-145.
24. Porcari, J.P., et al., Effect of Wearing the Elevation Training Mask on Aerobic Capacity, Lung Function, and Hematological Variables. Journal of sports science & medicine, 2016. 15(2): p. 379-386.
25. Ramírez-Moreno, J.M., et al., Mask-associated de novo headache in healthcare workers during the Covid-19 pandemic. 2020, Cold Spring Harbor Laboratory.
26. Rebmann, T., R. Carrico, and J. Wang, Physiologic and other effects and compliance with long-term respirator use among medical intensive care unit nurses. American Journal of Infection Control, 2013. 41(12): p. 1218-1223.
27. Roberge, R.J., et al., Physiological impact of the N95 filtering facepiece respirator on healthcare workers. Respir Care, 2010. 55(5): p. 569-77.
28. Roberge, R.J., J.-H. Kim, and J.B. Powell, N95 respirator use during advanced pregnancy. American Journal of Infection Control, 2014. 42(10): p. 1097-1100.
29. Roberge, R.J., J.H. Kim, and S.M. Benson, Absence of consequential changes in physiological, thermal and subjective responses from wearing a surgical mask. Respir Physiol Neurobiol, 2012. 181(1): p. 29-35.
30. Scarano, A., F. Inchingolo, and F. Lorusso, Facial Skin Temperature and Discomfort When Wearing Protective Face Masks: Thermal Infrared Imaging Evaluation and Hands Moving the Mask. International Journal of Environmental Research and Public Health, 2020. 17(13): p. 4624.
31. Scarano, A., et al., Protective Face Masks: Effect on the Oxygenation and Heart Rate Status of Oral Surgeons during Surgery. Int J Environ Res Public Health, 2021. 18(5).
32. Silke, S., et al., Corona children studies "Co-Ki": First results of a Germany-wide registry on mouth and nose covering (mask) in children. Research Square, 2021.
33. Smart, N.R., et al., Assessment of the Wearability of Facemasks against Air Pollution in Primary School-Aged Children in London. International Journal of Environmental Research and Public Health, 2020. 17(11): p. 3935.
34. Smith, C.L., J.L. Whitelaw, and B. Davies, Carbon dioxide rebreathing in respiratory protective devices: influence of speech and work rate in full-face masks. Ergonomics, 2013. 56(5): p. 781-790.
35. Tong, P.S.Y., et al., Respiratory consequences of N95-type Mask usage in pregnant healthcare workers—a controlled clinical study. Antimicrobial Resistance & Infection Control, 2015. 4(1).
36. Zhu, J., et al., Evaluation of rebreathed air in human nasal cavity with N95 respirator: a CFD study. Trauma Emerg. Care, 2016. 1(2): p. 15-18.
37. Zimmerman, N.J., et al., Effects of respirators on performance of physical, psychomotor and cognitive tasks. Ergonomics, 1991. 34(3): p. 321-334.
38. Bar-On, O., et al., Effects of Wearing Facemasks During Brisk Walks: A COVID-19 Dilemma. The Journal of the American Board of Family Medicine, 2021. 34(4): p. 798-801.
39. Driver, S., et al., Effects of wearing a cloth face mask on performance, physiological and perceptual responses during a graded treadmill running exercise test. British Journal of Sports Medicine, 2021: p. bjsports-2020-1.
40. Martellucci, C.A., et al., Inhaled CO<sub>2</sub> concentration while wearing face masks: a pilot study using capnography. medRxiv, 2022: p. 2022.05.10.22274813.
41. Walach, H., et al., Carbon dioxide rises beyond acceptable safety levels in children under nose and mouth covering: Results of an experimental measurement study in healthy children. Environmental Research, 2022. 212: p. 113564.
Infection Control Hazard
Infection Control Hazard through cross-contamination, risk compensation, pathogen retention, enhanced bacterial and fungal growth on or under the mask, and/or increased viral viability duration.
1. Chao, F.-L., Adolescents’ face mask usage and contact transmission in novel Coronavirus. Journal of Public Health Research, 2020. 9(1).
2. Chin, A.W.H., et al., Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe, 2020. 1(1): p. e10.
3. Chughtai, A.A., et al., Contamination by respiratory viruses on outer surface of medical masks used by hospital healthcare workers. BMC Infectious Diseases, 2019. 19(1).
4. Fisher, E.M., et al., Validation and Application of Models to Predict Facemask Influenza Contamination in Healthcare Settings. Risk Analysis, 2014. 34(8): p. 1423-1434.
5. Gund, M., et al., Contamination of surgical mask during aerosol-producing dental treatments. Clin Oral Investig, 2020: p. 1-8.
6. Luckman, A., et al., Risk Compensation during COVID-19: The Impact of Face Mask Usage on Social Distancing. OSF Preprints, 2020.
7. Luksamijarulkul, P., N. Aiempradit, and P. Vatanasomboon, Microbial Contamination on Used Surgical Masks among Hospital Personnel and Microbial Air Quality in their Working Wards: A Hospital in Bangkok. Oman Medical Journal, 2014. 29(5): p. 5.
8. Monalisa, A.C., et al., Microbial contamination of the mouth masks used by post-graduate students in a private dental institution: An In-Vitro Study. IOSR J Dent Med Sci, 2017. 16: p. 61-7.
9. Scarano, A., F. Inchingolo, and F. Lorusso, Facial Skin Temperature and Discomfort When Wearing Protective Face Masks: Thermal Infrared Imaging Evaluation and Hands Moving the Mask. International Journal of Environmental Research and Public Health, 2020. 17(13): p. 4624.
10. Yan, Y., et al., Risk compensation and face mask mandates during the COVID-19 pandemic. Scientific Reports, 2021. 11(1).
11. Zhiqing, L., et al., Surgical masks as source of bacterial contamination during operative procedures. J Orthop Translat, 2018. 14: p. 57-62.
12. Keri, V.C., et al., Pilot study on burden of fungal contamination in face masks: need for better mask hygiene in the COVID-19 era. Le Infezioni in Medicina, 2021. 36: p. 25-49
13. 1. Park, A.-M., et al., Bacterial and fungal isolation from face masks under the COVID-19 pandemic. Scientific Reports, 2022. 12(1).
Psychological Harms
Adverse user experiences, anxiety, sleep disturbance, concentration difficulty, interpersonal and relational impairment.
1. Carbon, C.-C., Wearing face masks strongly confuses counterparts in reading emotions. Frontiers in Psychology, 2020. 11: p. 2526.
2. Cheok, G.J.W., et al., Appropriate attitude promotes mask wearing in spite of a significant experience of varying discomfort. Infect Dis Health, 2021.
3. Köseoğlu Toksoy, C., et al., Headache related to mask use of healthcare workers in COVID-19 pandemic. The Korean Journal of Pain, 2021. 34(2): p. 241-245.
4. Li, Y., et al., Effects of wearing N95 and surgical facemasks on heart rate, thermal stress and subjective sensations. International Archives of Occupational and Environmental Health, 2005. 78(6): p. 501-509.
5. Mheidly, N., et al., Effect of Face Masks on Interpersonal Communication During the COVID-19 Pandemic. Frontiers in Public Health, 2020. 8.
6. Morgan, W.P., Psychological Problems Associated with the Wearing of Industrial Respirators: A Review. American Industrial Hygiene Association Journal, 1983. 44(9): p. 671-676.
7. Prousa, D., Studie zu psychischen und psychovegetativen Beschwerden mit den aktuellen Mund-Nasenschutz-Verordnungen [Study of psychological and psycho-vegetative complaints by the current mouth and nose protection regulations in Germany]. 2020.
8. Radonovich, L.J., Respirator Tolerance in Health Care Workers. JAMA, 2009. 301(1): p. 36.
9. Ramírez-Moreno, J.M., et al., Mask-associated de novo headache in healthcare workers during the Covid-19 pandemic. 2020, Cold Spring Harbor Laboratory.
10. Scheid, J.L., et al., Commentary: Physiological and Psychological Impact of Face Mask Usage during the COVID-19 Pandemic. Int J Environ Res Public Health, 2020. 17(18).
11. Silke, S., et al., Corona children studies "Co-Ki": First results of a Germany-wide registry on mouth and nose covering (mask) in children. Research Square, 2021.
12. Wong, C.K.M., et al., Effect of facemasks on empathy and relational continuity: a randomised controlled trial in primary care. BMC Family Practice, 2013. 14(1): p. 200.
Headaches
Range from minor to migraine; both de novo and exacerbation of pre-existing headaches. Severity increases with mask quality. Includes associated symptoms of nausea, dizziness, tachepynea, palpitation, fatigue, and cognitive impairment.
1. Bharatendu, C., et al., Powered Air Purifying Respirator (PAPR) restores the N95 face mask induced cerebral hemodynamic alterations among Healthcare Workers during COVID-19 Outbreak. Journal of the Neurological Sciences, 2020. 417: p. 117078.
2. Hajjij, A., et al., Personal Protective Equipment and Headaches: Cross-Sectional Study Among Moroccan Healthcare Workers During COVID-19 Pandemic. Cureus, 2020. 12(12): p. e12047.
3. Kisielinski, K., et al., Is a Mask That Covers the Mouth and Nose Free from Undesirable Side Effects in Everyday Use and Free of Potential Hazards? International Journal of Environmental Research and Public Health, 2021. 18(8): p. 4344.
4. Köseoğlu Toksoy, C., et al., Headache related to mask use of healthcare workers in COVID-19 pandemic. The Korean Journal of Pain, 2021. 34(2): p. 241-245.
5. Lim, E.C.H., et al., Headaches and the N95 face-mask amongst healthcare providers. Acta Neurologica Scandinavica, 2006. 113(3): p. 199-202.
6. Ong, J.J.Y., et al., Headaches Associated With Personal Protective Equipment - A Cross-Sectional Study Among Frontline Healthcare Workers During COVID-19. Headache, 2020. 60(5): p. 864-877.
7. Radonovich, L.J., Respirator Tolerance in Health Care Workers. JAMA, 2009. 301(1): p. 36.
8. Ramírez-Moreno, J.M., et al., Mask-associated de novo headache in healthcare workers during the Covid-19 pandemic. 2020, Cold Spring Harbor Laboratory.
9. Rebmann, T., R. Carrico, and J. Wang, Physiologic and other effects and compliance with long-term respirator use among medical intensive care unit nurses. American Journal of Infection Control, 2013. 41(12): p. 1218-1223.
10. Rosner, E., Adverse Effects of Prolonged Mask Use among Healthcare Professionals during COVID-19. Journal of Infectious Disease and Epidemiology, 2021. 6(3): p. 130.
11. Scarano, A., et al., Protective Face Masks: Effect on the Oxygenation and Heart Rate Status of Oral Surgeons during Surgery. Int J Environ Res Public Health, 2021. 18(5).
12. Silke, S., et al., Corona children studies "Co-Ki": First results of a Germany-wide registry on mouth and nose covering (mask) in children. Research Square, 2021.
13. Zaheer, R., et al., Association of Personal Protective Equipment with De Novo Headaches in Frontline Healthcare Workers during COVID-19 Pandemic: A Cross-Sectional Study. Eur J Dent, 2020. 14(S 01): p. S79-s85
Skin Damage
Includes physical irritation and trauma (e.g. itch, ulceration, desquamation, fissure, etc.), allergic reactions (e.g. contact dermatitis), and exacerbation of bacteriogenic dermatological issues (e.g. acne, some types of seborrheic dermatitis)
1. Bhatia, R., et al., Iatrogenic dermatitis in times of COVID-19: a pandemic within a pandemic. J Eur Acad Dermatol Venereol, 2020. 34(10): p. e563-e566.
2. Bothra, A., et al., Retroauricular dermatitis with vehement use of ear loop face masks during COVID-19 pandemic. J Eur Acad Dermatol Venereol, 2020. 34(10): p. e549-e552.
3. Foo, C.C.I., et al., Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome ? a descriptive study in Singapore. Contact Dermatitis, 2006. 55(5): p. 291-294.
4. Hua, W., et al., Short-term skin reactions following use of N95 respirators and medical masks. Contact Dermatitis, 2020. 83(2): p. 115-121.
5. Jacek C. Szepietowski, Ł.M.M.S.P.K.K. and B.-B. Rafał, Face Mask-induced Itch: A Self-questionnaire Study of 2,315 Responders During the COVID-19 Pandemic | Abstract | Acta Dermato-Venereologica. Acta DermatoVenereologica, 2020. 100.
6. Kisielinski, K., et al., Is a Mask That Covers the Mouth and Nose Free from Undesirable Side Effects in Everyday Use and Free of Potential Hazards? International Journal of Environmental Research and Public Health, 2021. 18(8): p. 4344.
7. Lan, J., et al., Skin damage among health care workers managing coronavirus disease-2019. Journal of the American Academy of Dermatology, 2020. 82(5): p. 1215-1216.
8. Li, Y., et al., Effects of wearing N95 and surgical facemasks on heart rate, thermal stress and subjective sensations. International Archives of Occupational and Environmental Health, 2005. 78(6): p. 501-509.
9. Liu, C., et al., Effects of wearing masks on human health and comfort during the COVID-19 pandemic. IOP Conference Series: Earth and Environmental Science, 2020. 531: p. 012034.
10. Matusiak, Ł., et al., Inconveniences due to the use of face masks during the COVID -19 pandemic: A survey study of 876 young people. Dermatologic Therapy, 2020. 33(4).
11. Radonovich, L.J., Respirator Tolerance in Health Care Workers. JAMA, 2009. 301(1): p. 36.
12. Rosner, E., Adverse Effects of Prolonged Mask Use among Healthcare Professionals during COVID-19. Journal of Infectious Disease and Epidemiology, 2021. 6(3): p. 130.
13. Scarano, A., F. Inchingolo, and F. Lorusso, Facial Skin Temperature and Discomfort When Wearing Protective Face Masks: Thermal Infrared Imaging Evaluation and Hands Moving the Mask. International Journal of Environmental Research and Public Health, 2020. 17(13): p. 4624.
14. Silke, S., et al., Corona children studies "Co-Ki": First results of a Germany-wide registry on mouth and nose covering (mask) in children. Research Square, 2021.
15. Szepietowski, J.C., et al., Face Mask-induced Itch: A Self-questionnaire Study of 2,315 Responders During the COVID-19 Pandemic. Acta Derm Venereol, 2020. 100(10): p. adv00152.
16. Techasatian, L., et al., The Effects of the Face Mask on the Skin Underneath: A Prospective Survey During the COVID-19 Pandemic. Journal of Primary Care & Community Health, 2020. 11: p. 215013272096616.
17. Veraldi, S., L. Angileri, and M. Barbareschi, Seborrheic dermatitis and anti-COVID-19 masks. J Cosmet Dermatol, 2020. 19(10): p. 2464- 2465.
18. Chaiyabutr, C., et al., Adverse skin reactions following different types of mask usage during the COVID-19 pandemic. Journal of the European Academy of Dermatology and Venereology, 2021. 35(3).
19. Montero-Vilchez, T., et al., Skin adverse events related to personal protective equipment: a systematic review and meta-analysis. Journal of the European Academy of Dermatology and Venereology, 2021. 35(10): p. 1994-2006.
20. Park, S.J., et al., Adverse skin reactions due to use of face masks: a prospective survey during the COVID-19 pandemic in Korea. Journal of the European Academy of Dermatology and Venereology : JEADV, 2021. 35(10): p. e628-e630.
21. Techasatian, L., et al., The Effects of the Face Mask on the Skin Underneath: A Prospective Survey During the COVID-19 Pandemic. Journal of Primary Care & Community Health, 2020. 11: p. 215013272096616.
Other
Includes other adverse secondary effects such as: communication impairment; rhinitis and vocal disorder; local changes to skin humidity and temperature; opthalmic Irritation and intraocular pressure increases; increased COVID-19 case fatality rate.
1. Fikenzer, S., et al., Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity. Clin Res Cardiol, 2020. 109(12): p. 1522-1530. 2. Gund, M., et al., Contamination of surgical mask during aerosol-producing dental treatments. Clin Oral Investig, 2020: p. 1-8.
3. Hua, W., et al., Short-term skin reactions following use of N95 respirators and medical masks. Contact Dermatitis, 2020. 83(2): p. 115-121.
4. Johnson, A.T., Respirator masks protect health but impact performance: a review. Journal of Biological Engineering, 2016. 10(1).
5. Kisielinski, K., et al., Is a Mask That Covers the Mouth and Nose Free from Undesirable Side Effects in Everyday Use and Free of Potential Hazards? International Journal of Environmental Research and Public Health, 2021. 18(8): p. 4344.
6. Li, Y., et al., Effects of wearing N95 and surgical facemasks on heart rate, thermal stress and subjective sensations. International Archives of Occupational and Environmental Health, 2005. 78(6): p. 501-509.
7. Liu, C., et al., Effects of wearing masks on human health and comfort during the COVID-19 pandemic. IOP Conference Series: Earth and Environmental Science, 2020. 531: p. 012034.
8. Matusiak, Ł., et al., Inconveniences due to the use of face masks during the COVID -19 pandemic: A survey study of 876 young people. Dermatologic Therapy, 2020. 33(4). 9. Radonovich, L.J., Respirator Tolerance in Health Care Workers. JAMA, 2009. 301(1): p. 36.
10. Scarano, A., F. Inchingolo, and F. Lorusso, Facial Skin Temperature and Discomfort When Wearing Protective Face Masks: Thermal Infrared Imaging Evaluation and Hands Moving the Mask. International Journal of Environmental Research and Public Health, 2020. 17(13): p. 4624.
11. Smart, N.R., et al., Assessment of the Wearability of Facemasks against Air Pollution in Primary School-Aged Children in London. International Journal of Environmental Research and Public Health, 2020. 17(11): p. 3935.
12. Heider, C.A., et al., Prevalence of Voice Disorders in Healthcare Workers in the Universal Masking COVID -19 Era. The Laryngoscope, 2021. 131(4). 13. Mheidly, N., et al., Effect of Face Masks on Interpersonal Communication During the COVID-19 Pandemic. Frontiers in Public Health, 2020. 8.
14. Rebmann, T., R. Carrico, and J. Wang, Physiologic and other effects and compliance with long-term respirator use among medical intensive care unit nurses. American Journal of Infection Control, 2013. 41(12): p. 1218-1223.
15. Silke, S., et al., Corona children studies "Co-Ki": First results of a Germany-wide registry on mouth and nose covering (mask) in children. Research Square, 2021.
16. Klimek, L., et al., A new form of irritant rhinitis to filtering facepiece particle (FFP) masks (FFP2/N95/KN95 respirators) during COVID-19 pandemic. World Allergy Organization Journal, 2020. 13(10): p. 100474.
17. Passali, D., et al., Effects of a Mask on Breathing Impairment During a Fencing Assault: A Case Series Study. Asian Journal of Sports Medicine, 2015. 6(3).
18. Janicijevic, D., et al., Intraocular pressure responses to walking with surgical and FFP2/N95 face masks in primary open-angle glaucoma patients. Graefes Arch Clin Exp Ophthalmol, 2021: p. 1-6.
19. Moshirfar, M., W.B. West, and D.P. Marx, Face Mask-Associated Ocular Irritation and Dryness. Ophthalmology and Therapy, 2020. 9(3): p. 397-400.
20. Mukerji, S., et al., Cost-effectiveness analysis of N95 respirators and medical masks to protect healthcare workers in China from respiratory infections. BMC Infectious Diseases, 2017. 17(1).
21. Rosner, E., Adverse Effects of Prolonged Mask Use among Healthcare Professionals during COVID-19. Journal of Infectious Disease and Epidemiology, 2021. 6(3): p. 130. 22. Gori, M., L. Schiatti, and M.B. Amadeo, Masking Emotions: Face Masks Impair How We Read Emotions. Frontiers in Psychology, 2021. 12(1541).
23. Green, J., et al., The implications of face masks for babies and families during the COVID-19 pandemic: A discussion paper. Journal of neonatal nursing : JNN, 2021. 27(1): p. 21-25.
24. Freud, E., et al., The COVID-19 pandemic masks the way people perceive faces. Scientific Reports, 2020. 10(1).
25. Saeidi, R., I. Huhtakallio, and P. Alku, Analysis of Face Mask Effect on Speaker Recognition. 2016. 1800-1804.
26. Fögen, Z., The Foegen effect: A mechanism by which facemasks contribute to the COVID-19 case fatality rate. Medicine, 2022. 101(7): p. e28924.
27. Stajduhar, A., et al., Face masks disrupt holistic processing and face perception in school-age children. Cognitive Research: Principles and Implications, 2022. 7(1).
SOURCES:
https://swprs.org/face-masks-evidence/
https://web.archive.org/web/20220208080223/https://www.thecompleteguidetohealth.com/masks.html
https://rumble.com/search/videos?q=Petty%20podcast
https://www.unmaskyourchild.com/
https://www.unmaskyourchild.com/the-mask-report-children-do-not-need-to-be-masked/
https://childrenshealthdefense.org/defender/masks-titanium-dioxide-cancer-cola/
https://childrenshealthdefense.org/defender/masks-sick-foegen-effect-covid-transmission-cola/
https://worldcouncilforhealth.org/resources/face-masks-the-risks-vs-benefits-for-children/
https://worldcouncilforhealth.org/resources/are-masks-effective-for-covid-19-what-the-science-says/
https://worldcouncilforhealth.org/resources/end-mask-mandates/
https://citizensforfreespeech.store/shop/free_speech/dr-blaylock-brochures/
https://aapsonline.org/mask-facts/
https://www.realmaskscience.com/references
Psy-op purposes of face cancelling:
Show fear of others: they are a potential threat to you
Create fear in others: you are a potential threat to them
Create psychological distancing
Dehumanization
Destroying individuality (our face makes us unique)
Massification (mass formation)
Reduce social interaction and communication
Induce social pressure towards the rebels and show massive compliance
Reinforce political and police authority
Increase acceptance of an unquestionable police state
SOURCE:
Comment from Professor Fred Nazar
James Roguski
The old system is crumbling, and we must build its replacement quickly.
If you are fed up with the government, hospital, medical, pharmaceutical, media, industrial complex and would like to help build a holistic alternative to the WHO, then feel free to contact me directly anytime.
JamesRoguski.substack.com/about
JamesRoguski.substack.com/archive
310-619-3055
All content is free to all readers.
All support is deeply appreciated.

























No comments:
Post a Comment